Abstract
Cardinali D and Della Starza I contributed equally
Foà R and Chiaretti S contributed equally
Background. Philadelphia-like acute lymphoblastic leukemia (Ph-like ALL) is a subgroup of B-lineage ALL characterized by a gene expression profile (GEP) that resembles that of Ph-positive ALL but lacks the BCR/ABL1 transcript. Ph-like ALL cases are characterized by CRLF2 overexpression, JAK-STAT pathway mutations, IKZF1 deletions and rearrangements involving cytokine receptors and tyrosine kinases. To identify Ph-like ALL cases, our group developed a predictive tool named "BCR/ABL1-like predictor", which is based on the quantification by quantitative PCR of 10 transcripts, specifically overexpressed by Ph-like ALL cases1.
ALL is the first neoplasm where the assessment of early response to therapy by minimal residual disease (MRD) monitoring is pivotal for guiding therapeutic choices. Real-time-quantitative PCR (RQ-PCR) of IG/TR gene rearrangements is the most widely used molecular method for MRD assessment.
The GIMEMA LAL2317 is a clinical trial designed for newly diagnosed adult B-lineage Ph-negative ALL that includes two cycles of blinatumomab in the consolidation phase. MRD is evaluated at established time points (TPs), the most important being TP2, i.e., after the first consolidation cycle with high-dose chemotherapy, and TP3, after the first cycle of blinatumomab.
Aim of this study. To refine risk relapse categories of Ph-like ALL cases based on their genomic features at presentation in combination with the MRD status.
Methods. We performed this sub-analysis on a cohort of Ph-like ALL cases enrolled in the GIMEMA LAL2317 protocol identified according to the BCR/ABL1-like predictor assay and that underwent a centralized comprehensive molecular screening at diagnosis by IG/TR gene rearrangements and targeted DNA/RNA sequencing.
MRD status was evaluated at specific TPs, i.e., TP2 and TP3, by RQ-PCR and digital droplet PCR (ddPCR).
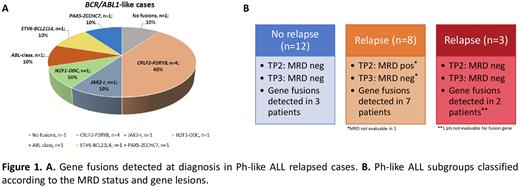
Results. A Ph-like profile was documented in 31/109 evaluable patients (28.4%); 11 of them (35.5%) experienced a relapse. By targeted RNA sequencing, 9/11 presented a gene fusion at presentation: in 4/9 a CRLF2-P2RY8 gene fusion was identified, whereas the remaining cases had PAX5-ZCCHC7, ETV6-BCL21L4, IKZF1-DDC, JAK2-r and ABL-class fusion in 1 case each (Figure 1A). The MRD status was evaluated at TP2 and TP3 by RQ-PCR in 23/31 patients: 15/23 were negative at both TPs, while 8/23 were positive at TP2 and negative at TP3; in the remaining 8 cases, MRD was not evaluated because of refractoriness (n=3), early death (n=2) or loss to follow-up (n=3). DdPCR analysis was performed in 9 patients and compared to RQ-PCR: 6/9 were concordant by both methods, while 3/9 resulted discordant with RQ-PCR being negative at TP3 while being positive by ddPCR.
On the basis of the Ph-like signature and MRD results, we defined 3 subgroups: i) Ph-like ALL cases (n=12, 39%) that did not relapse, being MRD-negative at both TP2 and TP3; 3 cases were positive for fusion genes; ii) relapsed Ph-like ALL cases (n=8, 26%) who were MRD-positive at TP2 but became MRD negative at TP3, with 7 harboring a fusion gene; iii) relapsed Ph-like ALL cases (n=3, 10%), always MRD-negative at both TPs, with 2/3 positive for fusion genes (Figure 1B). Finally, by flow cytometry analysis, available in 7 patients at relapse, 6 maintained CD19 positivity and only 1 proved CD19-negative.
Conclusions. Ph-like ALL patients tend to relapse early even after blinatumomab treatment and despite becoming MRD-negative. Relapse is not related to a mechanism of CD19 escape. Based on the gene fusions at presentation and on the MRD status, we could identify 3 subgroups of Ph-like ALL. These findings suggest that Ph-like ALL cases should be followed with different markers in addition to IG/TR, particularly in cases with well-defined fusion genes, who are at a very high risk of relapse. In this sense, a refined and rapid genetic characterization at presentation of Ph-like ALL cases is warranted for a more personalized and targeted patient management.
1. Chiaretti S et al., BJH 2018
Disclosures
Chiaretti:Amgen: Other: advisory board; Incyte: Other: advisory board; Abbvie: Other: advisory board; Gilead: Other: advisory board; Pfizer: Other: advisory board.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal